Firstly, my apologies for the length of this post, there’s a lot to tell. I’m posting rather than Avril because I have had absolutely nothing to do today!
(despite her being currently in the Cayman Islands)
Last week, Avril forgot to say that she was booked to have a heart scan on Monday 11th February. Very appropriate at the start of Valentine’s week.
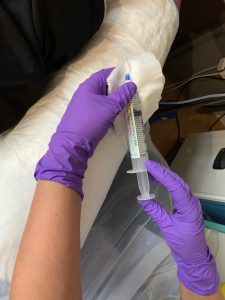
On the advice of the Nuclear Medicine Department, she drove herself to BMI Mount Alvernia Hospital for the scan because she had been warned that she would remain radioactive for a while and should not be near other people for at least six hours afterwards. The injection of the radioactive dye, via a cannula, was started and true to form her vein collapsed and she immediately felt faint, almost passing out.
Thankfully, she rallied and the scan was successfully completed. Thankfully also, she didn’t get a parking ticket for overstaying 45 minutes in her parking place.

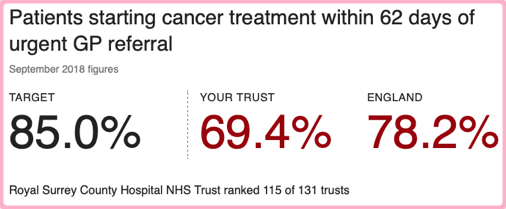
Despite not buying a Valentine’s Day card for me on 14th February, Avril’s scan has proved that unlike the Tin Man in the Wizard of Oz she does have a heart after all and fortunately the result of the test was completely normal. It will serve as a baseline during the next phase of treatment which can apparently affect the left ventricle of the heart, usually temporarily but occasionally permanently, hence the need for monitoring. She will have further scans every three to four months so her Consultant Oncologist can check how she’s being affected, if at all.
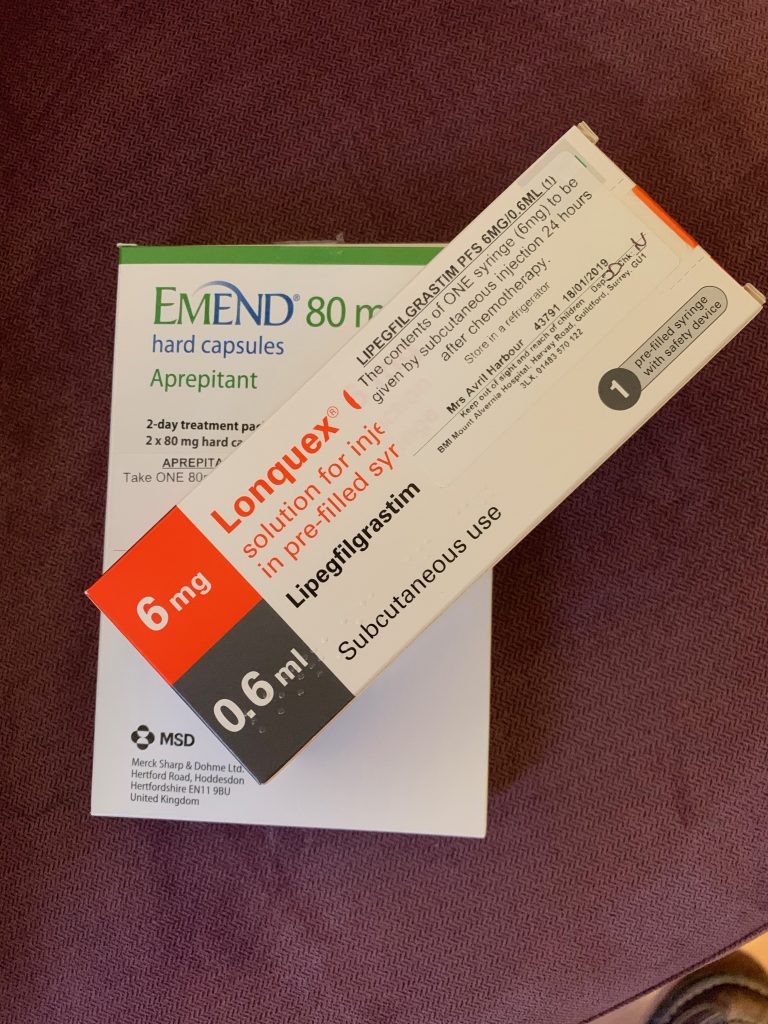
Generally Avril has not suffered any major side effects from the first cycle of the new regimen of Taxol chemotherapy; however last Sunday she felt very weary and listless and then made herself a bit depressed by reading in bed a few chapters of her book “The Complete Guide to Breast Cancer” which told her what awful things might be in store over the next few months.
She slept well that night and on Monday felt pretty much back to normal… except that she then found it difficult to sleep that night, so the pattern went all the way from needing to rest, to not being able to rest.
Tuesday in Guildford started with a frost but later turned into a lovely winter’s day; quite mild with a clear blue sky and sunshine. So between us we first cleaned the entire house and then blitzed the garden, trimming back all our shrubs and making it look a little like Hiroshima, 1945.
At 23:00, in the dark, we even managed to locate Avril’s lost FitBit at the bottom of one of the bags of garden refuse! We hope we didn’t disturb you Paul and Sarah…
On Wednesday, Avril went to a gentle exercise class at Spectrum Sports Centre and yesterday was a pretty busy day too, with “his and hers” dentist’s appointments and finally a delicious Valentine’s Day dinner thanks to the local Waitrose.

So Avril hasn’t exactly been relaxing, though she continues to pace herself carefully, following my sister Sue’s wise advice.
We knew that today would be long and tiring and as retirees it was very hard to wake up at 07:00 to the sound of the alarm clock. We arrived at BMI Mount Alvernia Hospital before 08:30 so this time there was plenty of parking space and no need to keep “feeding the meter”.
Our hectic day went like this, it’s simpler just to list what happened and it shows that there is never a dull moment in this journey:
| 08:30 | Arrival |
| 08:45 | Insertion of a tube into Avril’s Port-a-Cath by Nurse Lily |
| 08:45:30 | Ouch! That really hurt! |
| 08:46 | Bullseye! Second time lucky |
| 08:50 | Why is saline going in but no blood will come out? |
| 08:55 | Staff Nurse Ashley comes to check and says not to worry, that often happens, it’ll sort itself out |
| 09:00 | There’s 250ml of saline going in and blood is being taken by syringe from a vein in the back of Avril’s hand |
| 09:15 | A delicious breakfast for us both |
| 09:20 | A visit from our friend Elaine who’s working upstairs |
| 09:35 | Two Paracetamol tablets are taken (Tylenol to my U.S. readers) because the next infusion may cause a headache |
| 09:55 | Saline infusion complete |
| 10:40 | Reflexology by a volunteer from The Fountain Centre http://www.fountaincentre.org |
| 11:20 | Visit by the Consultant Oncologist to confirm that the heart scan was normal and that the “super-bug” MRSA blood test last week was negative |
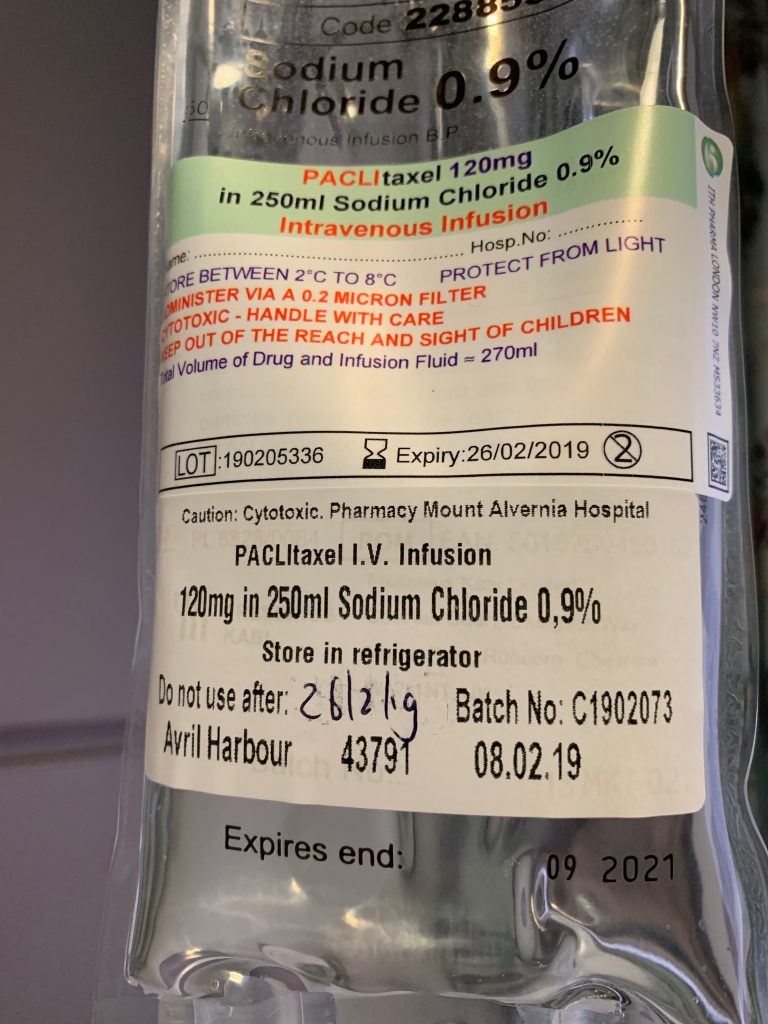
| 11:45 | Herceptin infusion commences. This first use is a “loading dose” of almost twice the normal strength |
| 12:30 | A delicious lunch |
| 13:15 | An hour's “rest” commences to check for any adverse reactions |
| 14:15 | Perjeta infusion commences which takes 90 minutes. This is another “loading dose”, double the normal strength |
| 15:45 | More saline and slightly more than an hour of observation |
| 16:25 | Avril’s suddenly feeling cold and her teeth start to chatter, despite the room heat being set to 27 Celsius (80 Fahrenheit) |
| 16:40 | Her temperature is taken and it’s 38 Celsius (100.4 Fahrenheit), so slightly elevated |
| 16:50 | The duty doctor arrives and after seeing Avril’s notes advises that this could be an effect of the Herceptin. More paracetamol is prescribed to lower her temperature and the Consultant Oncologist will make a decision shortly about whether the chemotherapy (Taxol) can go ahead |
| 17:00 | The Consultant’s decision is that, provided Avril feels she can cope, the chemotherapy can proceed. Avril says "Let's go for it" |
| 17:10 | The pre-meds are administered - Piriton and hydrocortisone |
| 17:40 | Avril’s temperature is taken again and it has risen to 39 Celsius (102.2 Fahrenheit). The chemotherapy needs to be abandoned as it would be unsafe to continue and of course more observation time is needed for her temperature to stabilise before we can go home |
| 19:25 | We set off home, 11 hours after our arrival but without completing the whole treatment. We will return for another try on Monday at 11:00 |
Avril is now feeling fine although her temperature is still a little elevated – but it’s going in the right direction.
One of us will post an update early next week, in the meantime have a good weekend!